Human blood successfully created in lab opens new era for regenerative medicine
Researchers have found a new way to produce human blood cells in the lab, mimicking the process in natural embryos. This is a great breakthrough, opening up new possibilities for regenerative medicine, using a patient's own cells to repair damaged tissue.

Scientists at the University of Cambridge have used human stem cells to create three-dimensional embryo-like structures that recreate certain aspects of early human development – including the production of blood stem cells.
Human blood stem cells, also known as hematopoietic stem cells, are immature cells that can develop into any type of blood cell, including oxygen-carrying red blood cells and many types of white blood cells important for the immune system.
The embryonic-like structures, dubbed 'hematoids' by scientists, were able to self-organise and begin producing blood after about two weeks of development in the lab - mimicking the development process in human embryos .
These structures differ from true human embryos in many ways, and cannot develop into true human embryos because they lack certain embryonic tissues, as well as the supporting yolk sac and placenta necessary for further development.
Hematoids have exciting potential to help us better understand blood formation during early human development, model blood disorders such as leukemia, and produce long-term blood stem cells for transplantation.
The human stem cells used to create the hematoid can be made from any cell in the body, meaning the method holds huge potential for personalized regenerative medicine in the future, by allowing the production of blood that is completely compatible with a patient's own body.
Self-organizing structure
The new human embryo model mimics the cellular changes that occur during early human development, when our organs and blood system begin to form.
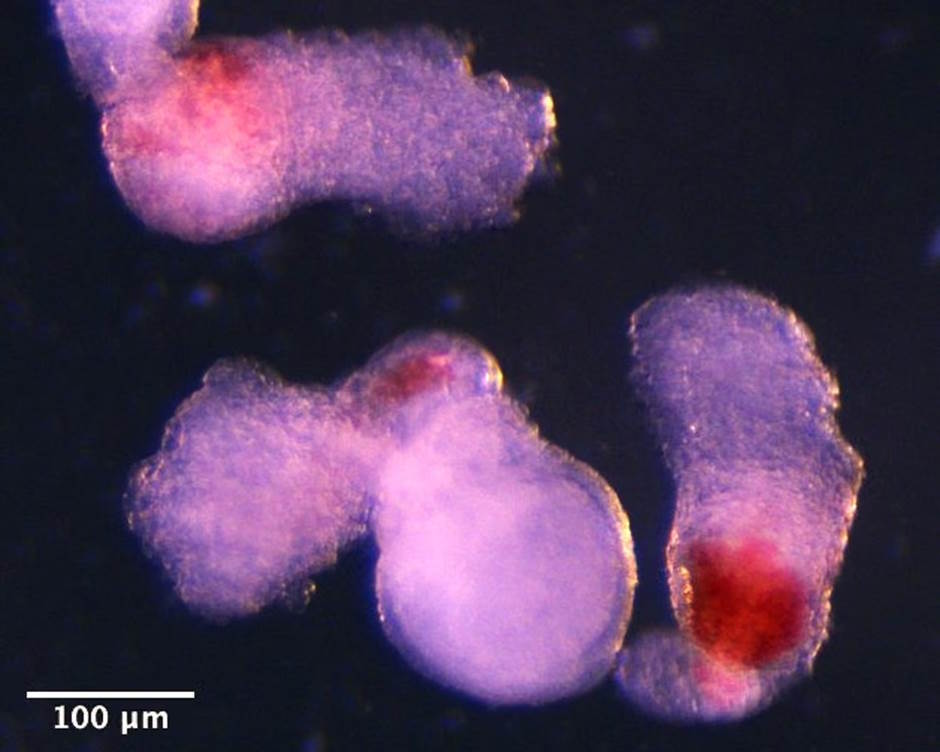
The team observed the emergence of three-dimensional hematoids under a microscope in the lab. By day two, they had organized themselves into three germ layers—called the ectoderm, mesoderm, and endoderm—the building blocks of the human body, which play a key role in shaping all organs and tissues, including blood.
By day eight, beating heart cells have formed. These cells eventually form the heart in the developing human embryo.
By day thirteen, the team saw patches of red blood appearing in the hematoids. They also developed a method to demonstrate that blood stem cells in the hematoids could differentiate into many different types of blood cells, including specialized immune cells, such as T cells.
Research results shed light on the reasons for early human development
Stem cell-derived embryonic models are important for improving our understanding of early human development.
The blood cells in the hematoid develop to a stage corresponding to the fourth to fifth week of human embryonic development. This very early stage of life cannot be observed directly in a real human embryo because the embryo has already implanted in the mother's uterus.
There are clear regulations governing the construction of stem cell-based human embryonic models, and all research modeling human embryonic development must be approved by an ethics committee before proceeding. This study has received the necessary approvals and the resulting paper has been peer-reviewed.
The scientists have patented the work through Cambridge Enterprise, the University of Cambridge's innovation arm, which helps researchers transform their work into globally leading economic and social products.